BACK TO RESEARCH WITH IMPACT: FNR HIGHLIGHTS
As the FNR marks 25 years since its creation, we highlight 25 examples of FNR-supported research with impact.
In Luxembourg alone, thousands of people are affected by cancer every year. Either by being diagnosed with it, or because a loved one is affected. In Luxembourg, Prof Dr Simone Niclou and Dr Guy Berchem have spent the last two decades advancing knowledge of and treatment for this disease that accounts for a quarter of deaths in the country.
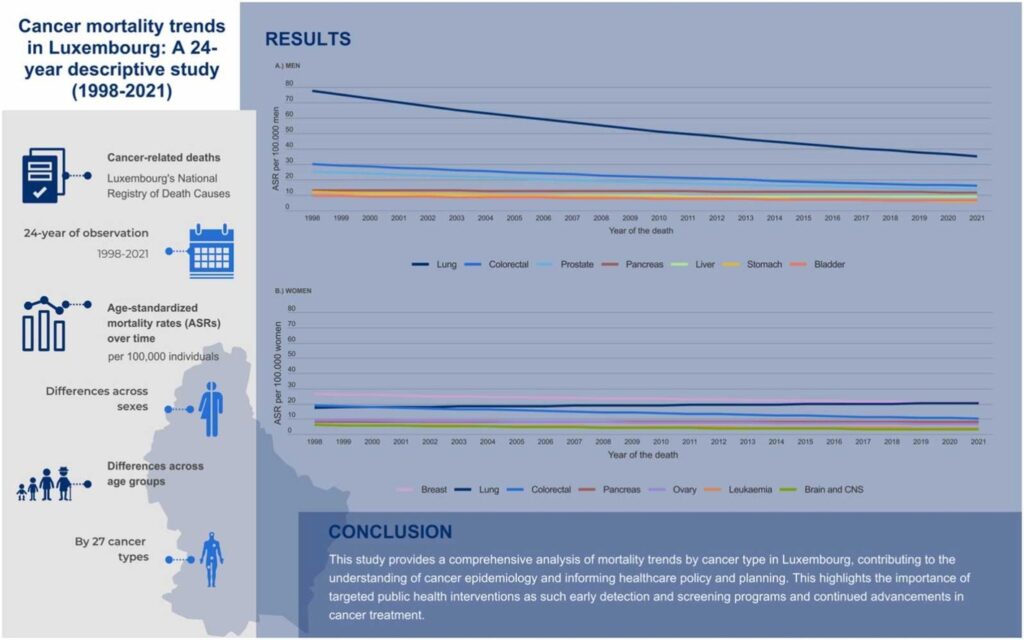
Around 3,000 people in Luxembourg are diagnosed with cancer each year. A recently published study from the Luxembourg Institute of Health, which analysed Luxembourg’s cancer-related deaths over 24 years, found that cancer deaths declined by 2.1% per year – proof that the many research efforts in the areas of earlier detection and better treatments are not in vain. New promising treatments, such as immunotherapy, are offering hope for increased survival in the future on the difficult quest to get this disease under control.
“In people below the age of 70, cancer is the first cause of death, and it constitutes a huge burden to our society. Treating or curing this disease would make an enormous impact on our lives and the economy of our countries. ”Dr Guy Berchem Medical oncologist (CHL), Associated Medical Director (Luxembourg Institute of Health)
Retrospective: A researcher and oncologist join forces to launch Luxembourg’s first cancer research lab
Around 2003, medical oncologist Dr Guy Berchem got his first FNR grant. Soon after he began the work to set up a cancer research lab at the CRP Santé, which later became the Luxembourg Institute of Health (LIH).
In 2005, Prof Dr Simone Niclou, returned to her home country Luxembourg and worked together with Prof. Rolf Bjerkvig, a close collaborator from Norway, to build up research on brain cancer. She became Head of the Department of Cancer Research in 2019 and stayed active in cancer research until 2023, when she took up the position of Vice-Rector for Research at the University of Luxembourg.
Since taking off her “researcher hat”, Dr. Anna Golebiewska, who co-lead the NORLUX Lab at LIH together with Niclou, has since taken over running the lab.
““Guy and I were actually, at the beginning, at the basis of establishing the Department of Cancer Research at the LIH. His lab was focusing more on blood cancer and my lab focusing on brain cancer. We shared a lot of enthusiasm and dynamism in setting up something new,” Simone Niclou explains. “Simone was very, very helpful. She's a wonderful scientist and together we could really make many things happen,” adds Guy Berchem. ”

The creation of these two labs, which later became a whole department at the Luxembourg Institute of Health (LIH), set in motion a wealth of research projects in Luxembourg that focus on all aspects of cancer research: Prevention, diagnosis and treatment.
Link between clinic and research essential
“ “Later, when we set up the clinical cohort on patient-based models, Guy was very instrumental in providing us clinical data of the patients,” Simone Niclou explains. “For a cancer researcher, it is important to have a relationship with the clinic. What we were able to do in CHL was to give the neuro- oncology lab of Simone Niclou this link and give her the data and samples from the patients that I had in my clinic. This is a very important part of the collaboration between clinicians and researchers,” Dr Guy Berchem adds. ”
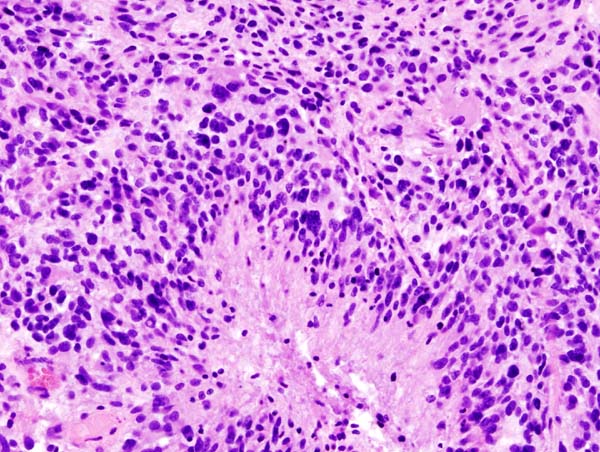
Glioblastoma, the most aggressive and resistant brain tumour
One of the cancers being investigated in Luxembourg is Glioblastoma, a type of brain cancer – the one Simone Niclou focussed on the most during her 18 years working in cancer research in Luxembourg.
Glioblastoma is the most aggressive and resistant of the primary brain tumours and is one of the deadliest cancers. Even with optimal management following diagnosis, the average life expectancy is only 14 months.
Research has found a link between this poor outlook and “pro-tumour” behaviour of the brain’s immune cells, microglia. Evidence is mounting that the tumour has developed complex molecular mechanisms to evade the immune system.
“Glioblastoma is a rare cancer – about 4 in 100,000 people are diagnosed with it every year, but many people I speak to know someone who has been diagnosed with or died of this cancer”, explains Simone Niclou.
Emily Iversen, Digital Communications Manager at the FNR, is one of those people.
“My father died of a Glioblastoma in 2011, in Luxembourg. Even though it was devastating for my family, my father lived for more than 5 years after his diagnosis, which only around 5% of patients do. I am grateful that advances in cancer research gave us more time with him. Guy Berchem was one of my father’s oncologists and the exceptional dedication and presence he showed has never been forgotten in my family. It means a lot to me to know that researchers, such as those in the team Simone Niclou led, have and are putting so much effort into researching this horrible cancer that still has so many unknowns.”
Refuting a widespread belief
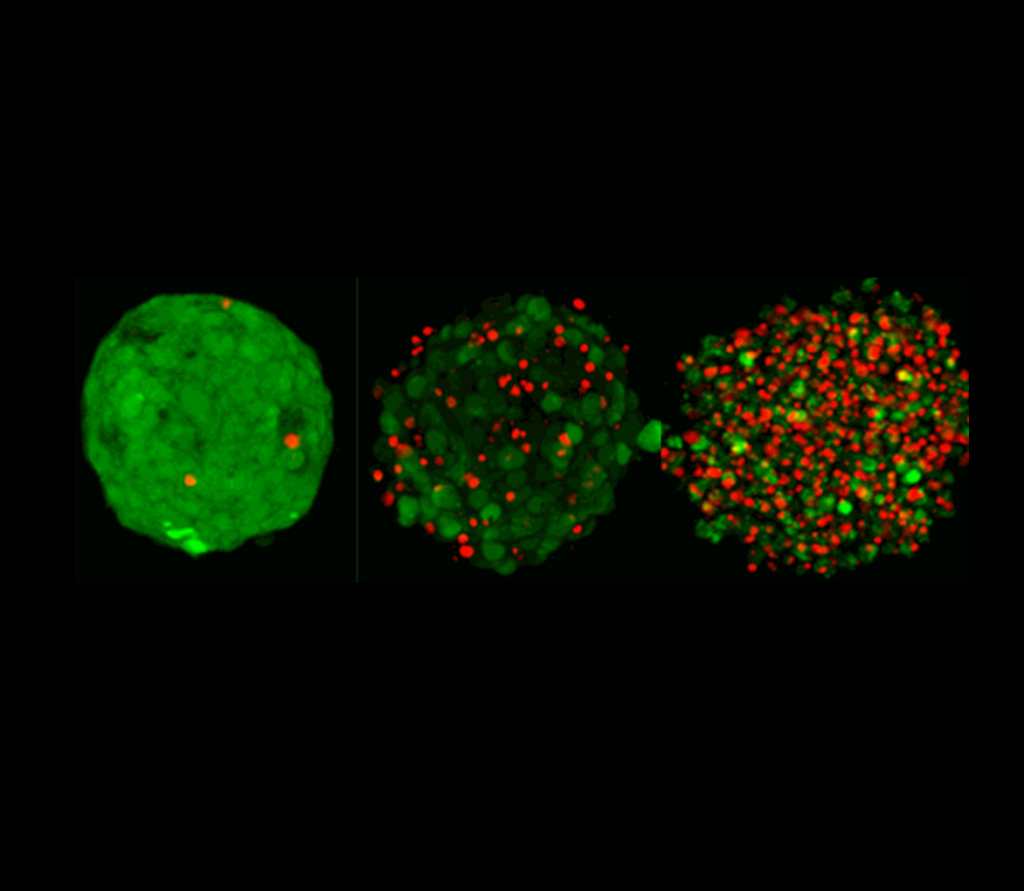
Over the two decades, Niclou led various projects that advanced the knowledge around glioblastoma. Her team for example played an important role in refuting a widespread paradigm amongst scientists of so-called ‘cancer stem cells’ in Glioblastoma, by showing that cancer cells are highly flexible and that the majority of these cells can adopt stem cell characteristics.
“Cancer cells basically act in disguise, which helps them survive and adapt to changing conditions in the brain. By the way, refuting a hypothesis is much more challenging than proving one, since you try to publish against the prevailing conviction,” Niclou explains.
Another major contrition from Niclou’s team is the establishment of complex patient-based preclinical models, such as organoids and PDOX mouse models.
“We set up and characterised a large cohort of such complex models which are internationally recognised and have fostered multiple international collaborations,” Niclou explains.
Tremendous development in diagnosis
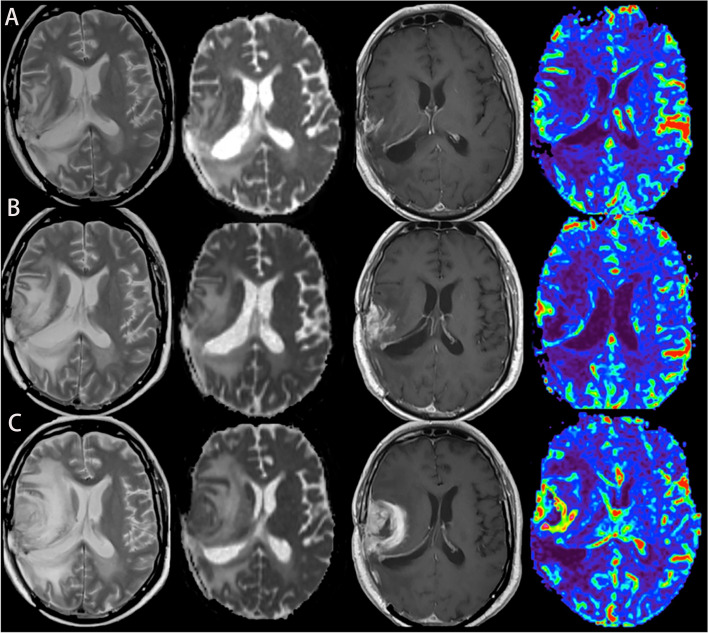
Niclou explains that there has been tremendous development in the last 10 – 20 years with regard to the diagnosis of brain tumours.

“This means that by now we can much better segregate the different types of brain tumours and hence align the best treatment for each affected individual. This is like identifying the different varieties of apples in a large basket, which is not trivial if you have to do it just by eye. Thanks to very precise yet high-throughput technologies, such as DNA sequencing and epigenetics, a more detailed identification became possible. Unfortunately, the treatment options have not yet advanced at the same rate. ”Prof Dr Simone Niclou Former co-leader NORLUX Oncology Lab (LIH), current Vice Rector for Research (University of Luxembourg)
In an FNR CORE funded project from around 2010, which focussed on anti-angiogenic treatment in Glioblastoma and was very topical at the time, the team tested a then novel treatment approach: blocking the formation of blood vessels in Glioblastoma, with the goal of “starving” the tumour.
“This treatment appeared very promising, yet in our complex models we could not see any beneficial effect on survival – a result that was later confirmed by two large multi-center clinical trials,” Niclou explains.
Immunotherapy, the promising emerging cancer treatment
Treatment is a focus of medical oncologist Dr Guy Berchem: cell death mechanisms and the reason why cancer cells do not die – the question: What is the reason for cancer treatment not working on certain patients? Why do the cancer cells survive, or why do they come back? A promising field of research for treatment in recent years has been immunotherapy, which Dr Guy Berchem has also devoted his research efforts to.
“The field of immune therapy has immensely evolved over the last 20 years, beforehand it was almost non-existent in cancer treatments. It is extremely important to develop new immune treatments if we want to win the battle against cancer. ”Dr Guy Berchem Medical oncologist (CHL), Associated Medical Director (Luxembourg Institute of Health)
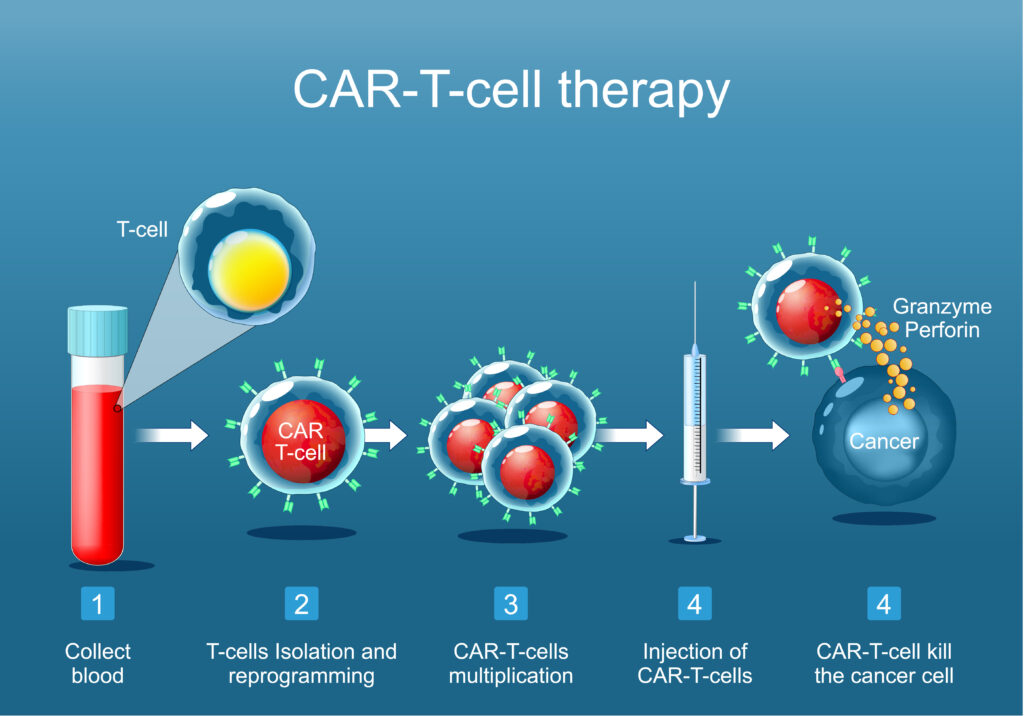
The question of why many cancer types do not respond to immunotherapy
Despite the promising therapy, it shares the common issue that also this treatment is not always effective in killing cancer cells.
“Cancer immunotherapy is a rapidly evolving field, but unfortunately many cancer types do not respond to this new treatment. Over the last years, we have been investigating the reasons why cancer cells or some patients do not respond to immunotherapy. We have discovered that the immune cell infiltration of the tumour, making them “hot” is probably at the center of this sensitivity or resistance to immune therapy,” Guy Berchem explains.
Berchem’s research has focussed on developing molecules that increase this immune cell invasion and thus makes them sensitive to immune therapy again.
“I want to better understand the mechanisms of immune therapy resistance, and some of our papers have resulted in showing new molecules as very promising future treatments of this situation. As developing new drugs is a very long process, our drugs are still being tested in clinical studies.”
Future challenges: Better treatments necessary & more patients to be enrolled in Luxembourg clinical studies
Looking toward the future, Dr Berchem expects his field will evolve in the direction of more integration of clinical and research applications, he stresses the need for more patient-based clinical studies in Luxembourg.
“We absolutely need to increase the number of patients enrolled in clinical studies in Luxembourg and we are currently working on that by establishing well organised clinical research center,” Berchem explains.


While Prof Dr Niclou sees improving treatment options as the biggest remaining challenge for researchers in the field, she is confident that the knowledge gained over the last years about the molecular and social behaviour of brain cancer cells will help pave this road. She explains that in the case of treatment for Gliomas, a promising new drug has recently been approved – the first new drug for this cancer in two decades.
“One brain tumour variety presents a novel mutation and a specific inhibitor has been developed against the mutant protein, a metabolic enzyme. This new drug, called Vorasidinib, has received FDA approval this year as a new medical treatment for this cancer type. It is the first new drug approval for gliomas in 20 years. Yet a lot remains to be done for the other types of brain cancer,” Niclou explains.
Impact goes beyond research
Both Dr Guy Berchem and Prof Dr Simone Niclou’s impact goes beyond research – it reaches the people around them.
“An important non-scientific impact which is not easily measurable is the direct impact on team members, on career development, and on the transfer of knowledge and values. As a research leader, you have the privilege to impact on the life of so many other researchers, e.g. PhD candidates, postdocs, technicians, young and senior research staff – which of course indirectly impacts again on research,” she concludes.
In 2021, the University of Luxembourg introduced a Bachelor in Medicine – Dr Guy Berchem is one of the lecturers, passing on his knowledge to the next generation.
FNR Awards awarded to Simone Niclou & Guy Berchem
In 2010, Simone Niclou, together with Uros Rajcevic (LIH), were awarded an FNR Award in the category Outstanding Scientific Publication for the paper “iTRAQ-based proteomics profiling reveals increased metabolic activity and cellular cross-talk in angiogenic compared with invasive glioblastoma phenotype”.
In 2012, Guy Berchem, together with Etienne Moussay (LIH), was awarded an FNR Award in the category Outstanding Scientific Publication for the paper ‘MicroRNA as biomarkers and regulators in B-cell chronic lymphocytic leukaemia – Proceedings of the National Academy of Sciences of the USA’.
In 2021, Simone Niclou and Anna Golebiewska (LIH), on behalf of a large team, were awarded an FNR Award in the category Outstanding Scientific Achievement for many years of research towards a better understanding and personalised treatment of brain cancer.
Simone Niclou on the impact of FNR funding
“Over the years, the FNR funding together with other types of funding were crucial to make my lab financially sustainable and productive. This allows to be recognised by the scientific community and build important partnerships. Thanks to the funding, I have been able to join several important world-wide consortia of researchers that pulled resources together to advance the field. E.g. by sharing tumour biopsies and molecular patient data with about 50 centers across the world, we contributed to the detailed molecular characterization of brain tumours. More recently, through another consortium we applied federated machine learning to brain tumour images which allowed a more precise tumour delineation, thereby helping surgeons and radiotherapists alike. Today, biomedical research is largely a multi-center effort and it is important to be able to contribute to the community.”
FNR-funded projects with Simone Niclou as main applicant
| Project title | Call year | FNR funding instrument |
| Lecture series in Cancer Research | 2018 | RESCOM |
| Lecture Series in Cancer Research | 2016 | RESCOM |
| Training in Cancer Biology: Focus on Tumour Escape Mechanisms | 2015 | PRIDE |
| Precision Medicine for Cancer | 2014 | RESCOM |
| Lecture series in Cancer Research | 2014 | RESCOM |
| Cancer Research Lecture Series | 2013 | RESCOM |
| Identifying tumor escape mechanisms after anti-angiogenic treatment in malignant gliomas | 2010 | CORE |
| Application of Cell Microencapsulation Technology to the Treatment of Brain Disorders | 2008 | CORE |
| Functional Validation of a New Therapeutic Strategy to Prevent Neurodegeneration and Subsequent Cognitive Impairment in Mouse Models of Alzheimer’s Disease | 2006 | BIOSAN-PROVIE (former funding instrument) |
FNR-funded projects with Guy Berchem as main applicant
| Project title | Call year | FNR funding instrument |
| Assessment the impact of selective ALDH1 inhibitors on tumor infiltrating lymphocytes and the therapeutic benefit of Immune checkpoint blockers | 2021 | BRIDGES |
| Telomere dysfunction in CLL and CML cells: involvement of topoisomeraseIIIalpha | 2010 | CORE |
| Detection of miRNAs in microvesicles isolated plasma of B chronic lymphocytic leukemia (CLL) patients | 2009 | CORE |
| Vaccination with Apoptotic B Leukemic Cells Loaded Antigen Presenting Cells in Chronic Lymphoid Leukaemia | 2001 | BIOSAN-PROVIE (former funding instrument) |
Related Funding Instruments
Related highlights
25 examples of research with impact: Smart materials for a sustainable future
As the FNR marks 25 years since its creation, we highlight 25 examples of FNR-supported research with impact. Since arriving…
Read more
25 examples of research with impact: Advancing AI and Computer Vision: From space tech to better healthcare
As the FNR marks 25 years since its creation, we highlight 25 examples of FNR-supported research with impact. Since arriving…
Read more
25 examples of research with impact: Understanding the evolution of the workplace in the digital era
As the FNR marks 25 years since its creation, we highlight 25 examples of FNR-supported research with impact. Active in…
Read more
25 examples of research with impact: Shaping the future of historical research in a digital age
As the FNR marks 25 years since its creation, we highlight 25 examples of FNR-supported research with impact Andreas Fickers…
Read more
25 examples of research with impact: Harnessing nature’s power for a sustainable future
As the FNR marks 25 years since its creation, we highlight 25 examples of FNR-supported research with impact. Since arriving…
Read more
25 examples of research with impact: Revolutionising nano-analytics for a complex world
As the FNR marks 25 years since its creation, we highlight 25 examples of FNR-supported research with impact. Since arriving…
Read more